For most policyholders, filing a claim is one of the few interactions they’ll ever have with their insurance company, which automatically places the claims process under scrutiny. The circumstances that typically necessitate filing a claim only serve to up the ante even further. Under these conditions, even the smallest of inefficiencies within an insurance company’s claims process can jeopardize the customer relationship, which is why it’s imperative that insurers dedicate themselves to improving the claims process and handling.
Why Is Improving The Claims Process Important?
At a time when most household budgets are stretched thin, it only makes sense that customers are being more thoughtful about their spending and want to dedicate their money to companies that make them feel valued. This mentality extends to the insurance industry.
According to a survey from Invoca — which included insurance customers — 76% of respondents said that they would stop doing business with a company after a single negative experience. By comparison, 63% of respondents said that they’d be willing to spend more for better customer service.
These figures clearly convey both the risk and reward inherent to claims process improvement: Deliver high-quality service to policyholders at a time of critical need and enjoy increased customer retention and potential revenue. Fall short of customer expectations and risk losing even once-loyal customers to competitors.
But customer satisfaction isn’t the only incentive for improving the claims process. Insurance companies that implement standardized claims handling practices and that automate key components of the claims process are able to enhance efficiency and achieve substantial cost savings. And by leveraging advanced technology, such as data analytics, insurers can more accurately assess customer behavior, prevent losses, and mitigate fraud.
Key Challenges of Claims Process Improvement
Although claims process improvement is a worthy endeavor, it can also be a significant undertaking. In order to increase their chances of success, it’s important that insurers be aware of the hurdles they’ll need to clear — hurdles such as:
Claims processes with multiple touchpoints
The claims process can be complex, spanning multiple stakeholders and decision points. With complexity comes risk — risk that claimants will have an inconsistent experience from one touchpoint to the next or that a pivotal step of the process may be unintentionally overlooked.
Automation can reduce much of this complexity, though insurers should be mindful not to completely replace human interaction with technology. While technology can streamline claims handling and processing, a human touch is still needed to ensure that claimants feel heard and understood and to make each interaction feel that much more meaningful.
Diverse customer needs
Customer expectations are at an all-time high, placing real pressure on insurers to perform. Leveraging technology to optimize insurance operations — including enhancing claims efficiency — can go a long way toward meeting those expectations. But in order to truly serve customer needs, insurers must tailor their service to the individual.
The insurance industry is in the midst of a real generational divide, with digital natives from younger generations eager to use innovative solutions and communicate through online channels. However, not all claimants are familiar — let alone comfortable — with using technology. A 2022 J.D. Power study shows that only 11% of P&C insurance customers fully utilize digital channels for all major steps of the claims process. Bearing this in mind, carriers must ensure that their claims process is designed for customers at all comfort levels and provide additional technical education and support as needed.
Disruption from smaller carriers
As we heard at Connected Claims USA 2022, smaller carriers are taking an unconventional approach to claims. These carriers are eliminating independent agents from the claims process, instead working directly with customers to settle claims. Many of these same companies are expanding their coverage into high-risk areas, offering proactive service, advising customers on whether to file a claim and holding their hand throughout the claims process.
Although it’s early yet, these unique methods have the potential to become industry trends, so insurance companies would do well to keep an eye out for potential disruption to the traditional claims process.
Emerging technology overload
Today’s insurers have access to a vast array of advanced technologies, the likes of which would have been unimaginable even a decade ago. But having access to technology and utilizing it effectively are two very different things, and carriers that blindly rush in run the risk of further complicating already intricate workflows and even make the claims process less efficient.
To get the greatest return on their investment and see actual claims process improvements, insurers must carefully vet insurtech providers, searching not just for qualified vendors, but for long-term partners. The same applies to the solutions themselves — before investing in the latest-and-greatest tools and technologies, carriers should first consider whether those systems meet their actual needs and whether they integrate with their own claims systems.
Seeking the next generation of claims adjusters
The insurance industry is in the midst of a talent shortage, as skilled employees retire and carriers struggle to fill vacancies. To prevent the loss of valuable knowledge and skills — particularly in regulatorily complex areas, such as worker’s compensation — many insurers have developed their own claims adjusting curriculum, created coaching and mentoring programs and even built entire departments dedicated to running company-specific training.
Beyond training, insurance companies are using automation to perform low-skill activities and investing in easily configurable software solutions that democratize coding. These solutions enable employees who might not have programming experience to design and build applications and workflows in support of claims processing.
Legacy claims systems
Carriers that choose to maintain their legacy claims systems — either because they see no immediate need to digitize or simply lack the budget to migrate their systems over — will always eventually see diminishing returns. The truth of the matter is that legacy claims systems are often cumbersome and costly to maintain, prevent carriers from adapting to changing customer requirements, and can impede IT innovation.
To see meaningful claims process improvements, insurance companies must first embrace digitization and all that it has to offer. Implementing a claims management system that can serve as a single point of truth for all claims data and claims-related interactions can open the door to future opportunities and more advanced technologies, enabling carriers to better evolve with the times.
How to Improve Claims Handling: 8 Tips
- Pay special attention to the pre-claims experience
Much of a customer’s claims experience is defined by what precedes it. From the moment a policyholder enrolls, they should feel cared for — nothing about the onboarding or pre-claims experience should be perfunctory. Insurers can impress by providing customers with self-service options or assisting them as they fill out insurance forms; being mindful to communicate through customers’ preferred channels; proactively notifying customers of errors and omissions in paperwork; and so on. - Make service delivery a top priority
When it comes to claims handling services, consistency is key. No matter what a customer’s particular needs, what prompted them to file a claim or where they find themselves in the claims process, it’s imperative that they receive a high level of service. Well-defined claims policies and protocols — documented in an enterprise content management system — and automated workflows can go a long way toward ensuring consistent service levels, even in the face of high caseloads and complex claims. - Take control of internal processes
Disparate and disjointed systems can create confusion for claims personnel, making it difficult for them to access the information they need to do their jobs or collaborate with other stakeholders. By investing in software that integrate with their existing claims systems, insurers can design seamless workflows that enable them to streamline internal processes, boost productivity and optimize claims efficiency. - Make the claims process as seamless as possible
The ability to settle and close out a claim as quickly as possible is essential to improving the claims process, and straight-through-processing is made far easier with the right automations. Depending on the particulars of the claim, an insurer may even be able to send a check out to the customer on the first call, resulting in a smooth and truly frictionless claims experience.
But expediency isn’t the only way to create a seamless claims experience. An insurer can capture a customer’s information at various stages of the claims process and store it in a centralized and secure location, effectively creating a single source of truth about that customer. Employees can then refer to this source of truth as they serve the claimant, which saves the customer from having to restate information, even as they interact with different claims personnel across different channels. The end result is omnichannel engagement and a truly seamless claims experience across all channels. - Provide routine training (and retraining)
Insurers can set adjusters, examiners, handlers, underwriters and other claims personnel up for success by providing them with a solid foundation — a foundation that consists of in-depth training on claims processing activities and company guidelines to ensure conformity and consistency. Insurers can also gauge the efficacy of training materials by defining key performance indicators for claims personnel and monitoring agents’ job performance against them.
Finally, carriers can reinforce key lessons by providing additional training as needed and should routinely re-evaluate existing curriculum to ensure that it aligns with current company objectives and industry best practices. - Invest in a data management and data modeling platform
Data management and modeling platforms are not only essential to automating claims processing workflows, they also enable insurers to develop a 360-degree view of customers — that is, a complete view of customers based on data aggregated from various touchpoints. Armed with this information, insurance companies can deliver a more personalized and thoughtful claims experience to each individual customer, forecast claims more accurately, streamline business operations and more. - Switch to digital claims
Digital claims refers to the collective tools and technology — including automation, artificial intelligence (AI), machine learning and data analytics — that enable insurers to manage the entire claims lifecycle using a single solution. By digitizing the claims process, insurance companies have the opportunity to increase efficiency, improve customer service, modernize operations and expedite claims processing. And by leveraging cutting edge technology such as AI and data analytics, insurers can unlock valuable insights from big data. - Form the right partnerships
When choosing insurtech providers, it’s important that carriers look to form long-term, meaningful relationships rather than just select a vendor to do the work and move on. The right provider should go the extra mile to understand an insurer’s key business objectives, have a clear sense of what’s possible using the latest technologies and act as an extension of an insurer’s team. By partnering with such a provider, an insurer can leverage technical integrations that streamline the claims process through automation and enable claims handlers to focus on supporting the customer, allowing for a superior customer experience.
Improve Claims Handling With Duck Creek Technologies
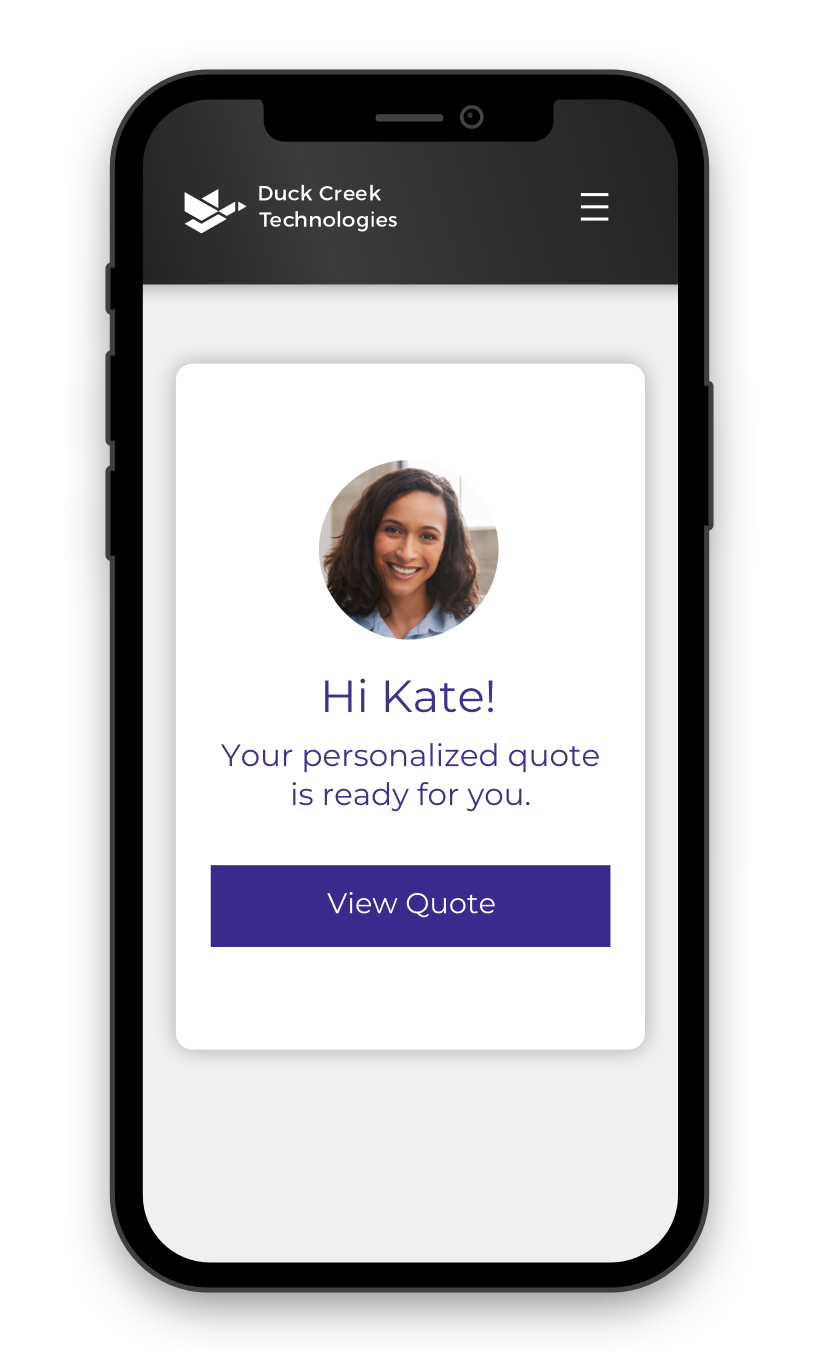
Duck Creek Claims is a comprehensive claims management system that helps insurers manage the entire claims lifecycle — from first notice of loss to settlement — in a single integrated solution. Through the use of automation, standardization and integration, Duck Creek Claims enables carriers to deliver fast and effective service, reduce claims cycle times, communicate with policy holders through their preferred channels and provide customers with high-quality service and support at their moment of greatest need.